When blood glucose levels fall below normal—typically below 70 milligrams per deciliter (mg/dL), hypoglycemia, also known as low blood sugar or low blood glucose, develops. Patients with diabetes are more likely to experience ‘dips’ in their blood sugar levels at night, which is referred to as nocturnal hypoglycemia.
What are some suggestions for preventing blood sugar decreases during the night?
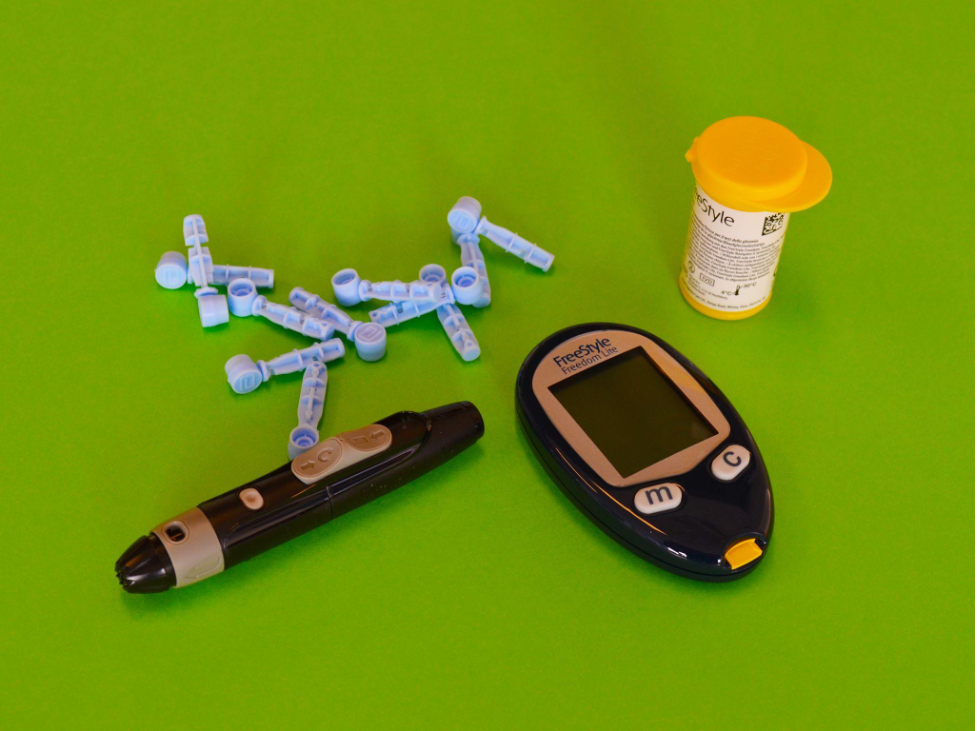
- Check that you’re at a safe level before going to bed. The only way to know whether you’re at risk, according to Sulay Shah, M.D., a board-certified endocrinologist, is to monitor your blood glucose levels, as there aren’t always clear indicators.
- Don’t forget to eat dinner. Dr. Shah recommends missing your rapid-acting insulin or blood sugar-lowering prescription, such as glipizide or glimepiride, if you aren’t eating dinner. “The aim here is to link your food with medicine,” he explains.
- Adjust your workout routine as necessary. Dr. Shah cautions that aerobic workouts, such as swimming or running on a treadmill, might cause your blood sugar to drop, but anaerobic exercises, such as weight lifting, can cause your blood sugar to rise. As a result, Dr. Shah recommends that people begin with anaerobic workouts and subsequently progress to aerobic exercises.
Check your blood glucose levels before working out. If your blood sugar is below 80 mg/dL, Dr. Shah recommends eating 10 to 15 grams of carbs before your workout and another 10 to 15 grams afterward. “As always, you must adjust your insulin properly,” he says. According to Dr. Shah, the body becomes more insulin sensitive 5 to 6 hours after exercising, and muscles will use blood sugar to counteract the stress of the activity.
RELATED: Glucofort supplement: Is it really worth it?
- Keep an eye on your alcohol consumption. If you notice that your blood sugar levels drop after a few beers or vodka soft drinks, Dr. Shah advises that you eat complex carbs in addition to the alcohol. According to Dr. Shah, blood sugar levels decline 3 to 4 hours after consuming alcohol.
- Recognize your risk factors. Certain patients, such as the elderly and those suffering from renal or hepatic disease, should double-check that their glucose levels are not excessively tightly regulated.
What is the best way to deal with hypoglycemia?
Hypoglycemia treatment includes both immediate actions to raise blood sugar levels as well as subsequent treatment or medication dose adjustments to prevent a recurrence.
To quickly elevate your glucose level, Dr. Shah recommends consuming 15 grams of carbohydrates and then monitoring your glucose level 15 minutes later.
Carbohydrates that act quickly include:
- 4 tablets of glucose
- Fruit juices in 4 oz
“Repeat these actions every 15 minutes until your blood sugar is higher than 70 mg/dL,” he says. Dr. Shah adds that once your blood sugar level has normalized, you should have a snack or perhaps a full meal to maintain that balance.
“You could need a glucagon infusion if your adverse effects are severe and you can’t swallow,” he explains.
Dr. Shah notes that modifying prescription regimens and dosages, as well as adjusting your meal patterns, might help prevent further hypoglycemic episodes.
What are the benefits of treating hypoglycemia?
Patients can put themselves at risk for a variety of medical complications if hypoglycemia episodes are frequent and untreated, according to Dr. Shah.
- Impairment of cognition
- Weakness or dizziness are two symptoms that you may experience
- The illness of the heart and blood vessels
- Controlling blood sugar levels is difficult
What symptoms do you look for if you have hypoglycemia?
As a result of nighttime hypoglycemia, a person may frequently wake up in the middle of the night. However, in some cases, people can tell if they have hypoglycemia while sleeping if they notice the following symptoms:
- I awoke with a headache
- I’m sweating as I wake up
- Experiencing unusual levels of fatigue throughout the day
- Anxiety or palpitations in the heart
- Feeling disoriented, dizzy, or shaky
Aside from diabetics, who else can be impacted by hypoglycemia?
Diabetics are more likely to have hypoglycemia, according to Dr. Shah. Non-diabetics, however, such as those with carbohydrate sensitivities or those who have undergone gastric bypass surgery, may be in danger of getting hypoglycemia, according to the expert.
Is there any new technology that can help prevent hypoglycemia?
“We are fortunate that, because to technology like continuous glucose monitors, we can now foresee hypoglycemia and avoid it,” Dr. Shah says. He also mentions that improved insulins are on the market to assist reduce hypoglycemic episodes.
Dr. Shah says, “One of our obligations as your doctor is to educate each patient about diabetes self-management and establish a particular treatment plan.” “If you self-manage your disease, you will genuinely feel empowered to take charge of your health.”
Resources:
The National Institute of Diabetes and Digestive and Kidney Illnesses is a government institution dedicated to researching diabetes and associated digestive and kidney diseases.
The material provided is for educational purposes only and should not be used as a substitute for medical advice. For individual care, always consult your doctor.

